Teilen:
Take it offline!
This Education in Motion resource is also available as a printable PDF.
Download PDF
The term "microclimate" was coined in the 1950s to describe any climatic condition in a relatively small area. Historically, the term has been used in a geographical, meteorological, or topographical context, but as of late it has made its way into the complex rehab industry to describe the mini-atmosphere of increased skin temperature and level of moisture at the seating interface.
Because of their limited mobility and sensation, wheelchair users are at risk for tissue injuries. We've known for decades that pressure and shear are clear culprits in these injuries, but continued research is determining that higher skin surface temperature and moisture are also contributing factors and management of this climate is also critical in healthy skin promotion.
Preventative Strategies
There are steps that caregivers and wheelchair users should take to manage the microclimate.
- Repositioning and weight shifts: these are essential in allowing improved airflow and moisture dissipation.
- Maximize pressure distribution: pressure itself may also lead to increases in skin temperature.
- Increase the heat dissipation away from the seated surface.
During the seating assessment, consideration of both the cushion design and materials needs to occur in order for the clients to effectively use these strategies.
- Consider the cushion materials:
- Is the cushion full contact, form fitting, and immersive? This type of cushion might reduce airflow - if so, more heat reduction strategies may be required.
- Is the cushion able to dissipate heat appropriate to the client and climate?
- Consider "active cooling strategies" provided by cushion material with the more "at-risk" clients.
- Consider cushion cover materials that optimize airflow with the more "at-risk" clients:
- Is it able to passively dissipate heat appropriate to the client and climate?
- Does it have the necessary wicking capability?
- What is the permeability of the cover material?
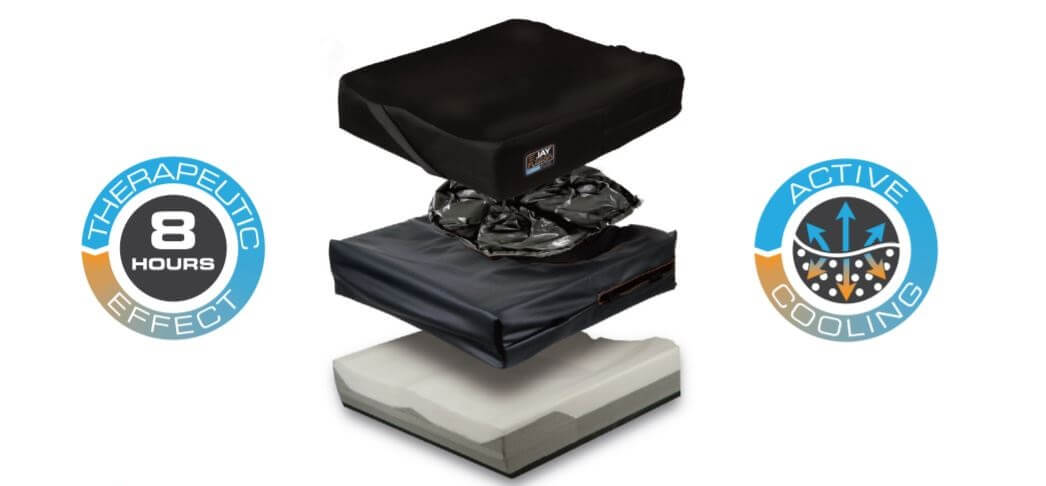
JAY Fluid® with Cryo™ Technology
This technology helps protect clients from pressure and shear injuries while addressing the risks inherent in heat and moisture. By addressing all four components of skin integrity management (pressure, shear, heat, moisture), JAY Fluid with Cryo Technology offers the highest degree of skin protection available on the market. The innovative CryoFluid offers an active method of keeping the cushion surface cooler. This technology helps to decrease heat and moisture at the cushion interface for up to 8 hours.
It's not magic. Just physics that work.
At the heart of the Cryo Technology are millions of microbeads filled with paraffin wax. As heat from the user moves into this fluid, it's absorbed by these microbeads and the wax inside actively begins to melt. The beads also contain graphite which draws the head down into the bladder, away from the user until the wax inside each microbead is melted. This active cooling process can last for up to 8 hours. During this time, the user's skin surface is cooled to a therapeutic temperature range.
The JAY Fluid with Cryo Technology provides wheelchair users skin protection across all of the risk factors: pressure, shear, moisture, and heat.